The Westview School Blog
Progress, Not Perfection: Understanding Growth in Neurodivergent Learners

When Ceara Wainright-Herod, Upper School Principal at The Westview School, addressed parents at a recent Westview EDU, she began with a simple question: What does progress really mean?
The answer, she suggested, has little to do with report cards. With nearly two decades of public education experience, Herod has worked with students across the autism spectrum, neurodivergent and neurotypical learners alike. One message, she says, has remained constant: growth differs for every child and rarely follows a straight line. Her Westview EDU session, "Progress, Not Perfection: Understanding Growth in Neurodivergent Learners," directly challenged the common belief that progress is only about grades, reinforcing that growth at Westview is about the whole child.
Beyond the Report Card
“Dictionary.com defines progress as growth and development, continuous improvement, a movement toward a goal,” Herod said. “Nowhere in that definition do you see the word ‘grades.’ Nowhere does it say ‘academics.’”
For many parents, grades carry enormous weight. A low test score can cause worry; a good report card offers reassurance. Herod believes equating grades with progress overlooks how children, especially neurodivergent ones, develop.
“There are so many skills your child is building that don’t show up on a report card,” she said. “Independence. Confidence. Curiosity. Emotional regulation. Problem-solving. Those are real gains. They deserve celebration.”
The Myth of the Straight Line
One important part of Herod’s message was the reminder that no child grows in a straight, predictable trajectory.
“Growth includes plateaus, regressions, and spurts,” she said. “That’s not a flaw, that’s development.”
She encouraged parents to recall their own school years: subjects that came naturally, years that were a struggle, moments when understanding clicked. Children experience the same uneven progression. Neurodivergent learners may show this more, but the pattern is universal.
“A single low grade isn’t the story,” she said. “It’s one data point in a much bigger picture.”
Three Lenses for Understanding Growth
Westview uses a holistic, strength-based model to understand student growth, which Herod believes offers a more accurate and compassionate view. The model includes three domains:
ACADEMIC GROWTH: This includes the traditional markers such as reading, writing, and math, as well as the quieter signs of learning: beginning an assignment independently, asking questions, showing persistence, and building comprehension over time.
“Academic growth isn’t just the score,” Herod said. “It’s effort, curiosity, and the willingness to try again.”
SOCIAL-EMOTIONAL GROWTH: This area encompasses emotional regulation, self-awareness, confidence, and peer relationships. For many neurodivergent learners, these skills take time to develop.
“When children don’t know something, we teach,” Herod emphasized. “That includes how to deal with frustration, how to express emotions, and how to calm their bodies and minds. These are learned skills.”
EXECUTIVE FUNCTIONING: Organizing materials, managing transitions, following routines, and using coping tools are key here.
Herod recalled watching Westview Middle School students confidently open their lockers this morning, something that had taken weeks of practice and patient guidance.
“It was incredible to witness,” she said. “Routine, structure, and repetition work. When students succeed, their pride is enormous.”
The Role of Discomfort in Growth
Herod repeatedly emphasized: growth is uncomfortable for children and adults.
She shared several quotes with the audience, including Brian Tracy’s well-known line, “Growth and comfort do not coexist.”
She explained that children resist new challenges not because they can't succeed, but because the discomfort can be overwhelming.
“Those big reactions you see? The protests, the tears? That’s fear,” she said. “They don’t yet have the words to say, ‘This scares me’ or ‘This is hard for me.’”
Parents can help their children manage discomfort by modeling coping strategies.
“Tell your kids, ‘I’m nervous about a meeting today, so I’m taking deep breaths,’” she suggested. “Show them what managing big feelings looks like. That vulnerability is powerful.”
Rethinking Assessment
Twice a year, Westview uses standardized MAP Growth assessments to gather academic data, but Herod urged parents not to put too much weight on the scores.
“These tests aren’t designed specifically for neurodivergent learners,” she explained. “Some students sit through 45 questions in one session. If they’ve had a tough morning, if they’re distracted, if they’re overwhelmed, that score isn’t representative of their true understanding.”
Instead, the school emphasizes teacher observations, student reflections, and classroom work samples for a complete picture of progress.
“Tests matter,” she said, “but they don’t define your child.”
A Partnership Between Home and School
Herod stressed the importance of partnership: parents know their children best, and teachers see them in structured settings. Together, families and educators provide continuity that helps students thrive.
She encouraged parents to share what works at home, ask questions during conferences, and communicate openly with teachers about concerns.
"We are a village," she said. “Your insight helps us support your child, and ours helps you support them at home. Working together, students make meaningful progress.”
A Final Story
Herod ended with a personal story. At four, she struggled with separation, sensory overwhelm, and fear, crying daily at her first school as staff grew frustrated.
“I wasn’t dramatic. I wasn’t a troublemaker. I was anxious,” she said. Her mother moved her to another school where she felt safe and welcomed. She never cried again.
"I share that to show what safety and belonging can do for a child," she said. “That's what we want for your children at Westview: a place where they feel loved, supported, and celebrated on all days.”
The Message Parents Took Home
By the end of the session, one message stood out: progress is not about achieving perfection, but about each child's unique, steady growth at their own pace.
“Your children are not victims of their challenges,” Herod said. “They are victors. And every day, we see their victories.”
--
Ceara Wainwright-Herod, M.Ed. is the Upper School Principal at The Westview School. She has over 18 years of experience in public education, having served as a teacher, specialist, and assistant principal in public school system. Her work is grounded in student-centered learning and inclusive leadership. Ceara holds a master’s in Educational Leadership from the University of Houston–Victoria and has extensive experience supporting students across the autism spectrum and has collaborated with families and specialists to design individualized plans that meet each learner’s needs.
This blog post was adapted from the presentation given during WestviewEDU on Thursday, November 13, 2025. WestviewEDU is an education series presented by The Westview School for parents and caregivers of children with autism. For a complete list of WestviewEDU sessions remaining for the 2025-2026 academic calendar year, visit The Westview School online.
Finding Strength Together: The Effectiveness and Benefits of Parent Support Groups

The day-to-day challenges of living with a neurodiverse child may lead to tremendous amounts of isolation and pressure that not many other parents understand. Some parents have been buried under this pressure for so long that we need to be reminded that support groups can be a powerful source of help for families and enable our parents to learn and build hope for the future. I am happy to start by saying that there is a significant list of benefits when it comes to parent support groups. I will be focusing on my top four benefits, which are a sense of community, building confidence, emotional support, and improved mental health.
Building a Sense of Community
A sense of community involves many bonding factors since you will be surrounded by other parents of neurodiverse children who understand your journey. Either these parents will be currently sharing your experiences, or you will be able to get a glimpse of what the future holds. This is also an opportunity to build a support network that can result in enduring lifelong friendships and connections that extend beyond the meetings. These relationships can positively impact the entire family, providing valuable experiences for both parents and children. Support groups enable parents to share information with one another, such as information about therapies or new programs, stories, and experiences which will broaden their access to resources.
Gaining Confidence and Resilience
Building self-confidence in parents can lead to greater resilience which then improves parent-child interactions. Therefore, active participation in support groups can lead to acquiring more profound comprehension of one’s own thoughts and emotions, as well as those of other individuals. This heightened self-awareness can contribute to increased confidence and improved parenting skills since you are sharing and learning in a supportive environment without fear of judgment. Refined parent skills lead to more positive child behaviors. The impact can be extraordinary, extending from the home to the classroom. Parents often witness the development of improved communication and cooperation overall.
Finding Emotional Support and Validation
Emotional support is a key component in our groups. First and foremost, parents feel less isolated and more understood. This fosters a sense of belonging and validation, which is essential for parents who are feeling overwhelmed or unsure of their parenting abilities. The opportunity to engage in conversations with other parents who share similar experiences enables parents to receive assurance and understanding. This may be the only environment where parents can openly share their challenges, shame, or embarrassment and receive empathy and encouragement from their peers. Parents may also receive practical advice that can leave a positive lasting impact.
Improving Mental Health Through Self-Care
Parent support groups can be seen as a form of self-care that improves your mental health. We can simply start by pointing out that this is a moment in time that you have intentionally carved out so that you can focus on yourself, which in turn will be beneficial for your whole family. There is a direct relationship between negative psychological health symptoms and physical health symptoms. This is also a reminder that your children will mirror your levels of stress, and you will model for them how to handle stressors. Therefore, by attending these groups and actively participating in discussions and activities, parents can effectively reduce stress and anxiety, leading to improved overall well-being for themselves and their families. I have witnessed the power of these support groups because of the power within each of our parents. It is a reminder that we are not alone, and it is a place to find hope and humor among supportive individuals who understand. We hope that you can take advantage of a support group and extend your community.
----
Mimi Le, M.A., LMFT, LPC is a Licensed Marriage and Family Therapist and a Licensed Professional Counselor. She provides therapy and consultations for adults, parents, siblings, children, families, and groups. She received her Bachelor of Arts Degree in Art History from Baylor University and earned her Master of Arts Degree in Family Therapy from the University of Houston – Clear Lake. She specializes in autism spectrum disorder, trauma- and stressor-related disorders, anxiety disorders, depressive disorders, interpersonal relationships, and multi-generational and cultural matters. She also provides parent-coaching and is the Clinical Director of The Stewart Center at The Westview School.
Opportunity for Westview Families: Texas Education Savings Accounts
A New Option for Families at The Westview School
Starting in the 2026–2027 school year, Texas families will have a new way to help pay for private and specialized education. The Education Savings Account (ESA) program, created through Senate Bill 2 and signed into law by Governor Greg Abbott in May 2025, sets aside $1 billion in public funds to support school choice across the state.
What Are Education Savings Accounts?
ESAs provide eligible families with access to state-managed accounts that can be used for education expenses outside the public school system. That includes tuition at private schools and other specialized programs such as The Westview School.
Westview is closely following how the program is being rolled out and will keep Westview families informed as more details become available. Our team will be here to help with updates, questions, and guidance on the application process.
How Much Can Families Receive?
Depending on eligibility, families may receive:
$2,000 per child for homeschooling or non-accredited private education
$10,000 per child enrolled in accredited private schools
$11,500 to $30,000 annually for children with disabilities, based on individual evaluations
Unused funds roll over from year to year as long as the student remains eligible.
What Can ESA Funds Be Used For?
ESA funds can be applied to a broad range of approved educational expenses, including:
- School tuition and fees
- Uniforms and meals
- Textbooks and instructional materials
- Therapies and interventions for special needs
- Online courses or tutoring
- Transportation and testing services
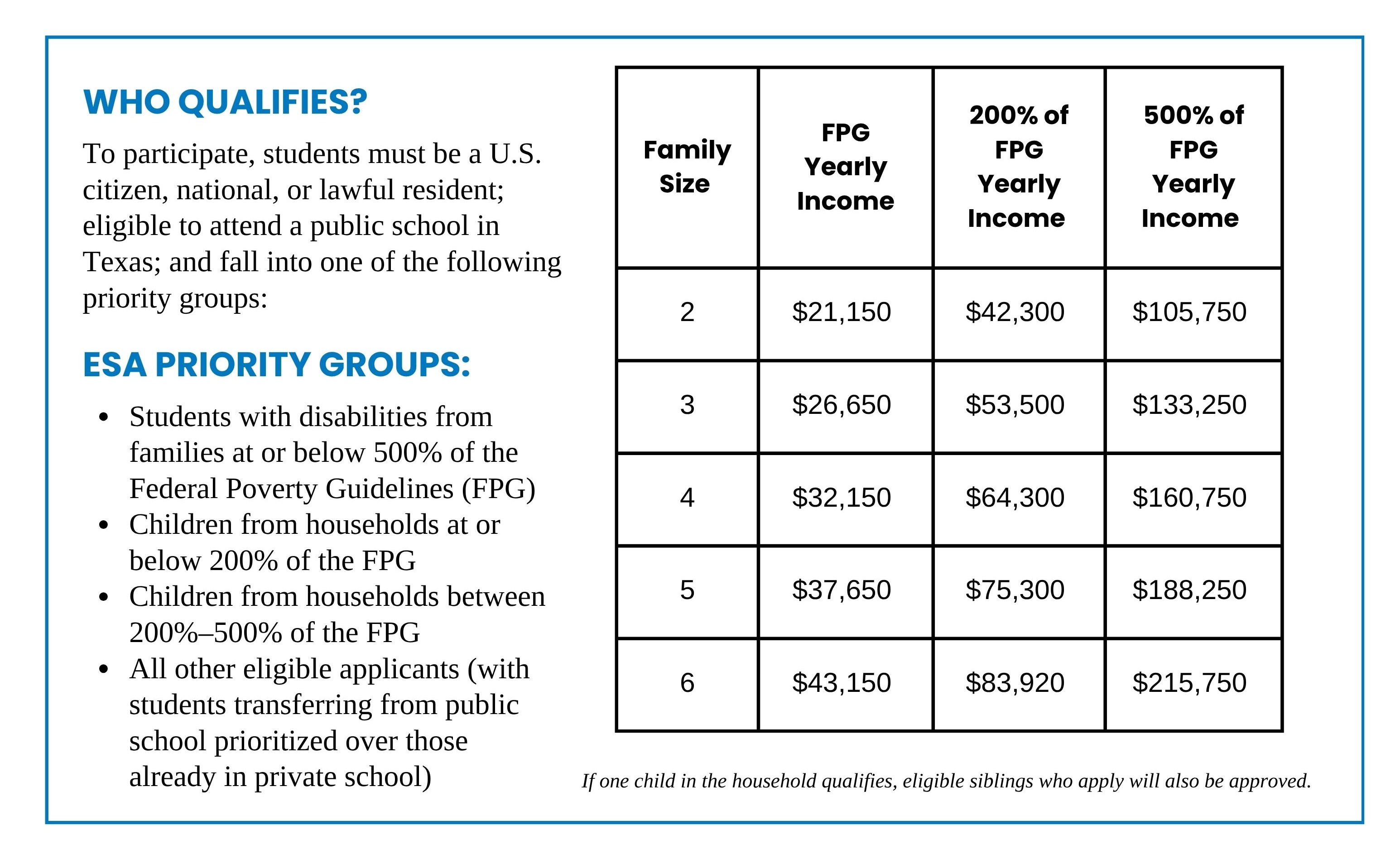
WHO QUALIFIES?
To participate, students must be a U.S. citizen, national, or lawful resident; eligible to attend a public school in Texas; and fall into one of the following priority groups:
What This Means for Westview Families?
The ESA program could be a big help for many Westview families. With funding amounts ranging from $11,500 to $30,000 per student, the program has the potential to alleviate the financial burden of tuition and related expenses. For families already navigating the costs of specialized education, this kind of support could make a real difference.
As awareness of the ESA program increases, we may see a growing interest in our school. That said, our admissions process isn’t changing. Westview will continue to focus on what matters most: making sure every student we accept is a strong fit for our program and that we can fully support their needs. Our mission remains the same, creating a supportive, developmentally appropriate space for children with autism to learn and thrive.
final thoughts
The ESA program represents a game-changing opportunity for Texas families. For those at Westview, it may offer meaningful financial help while allowing students to benefit from the kind of tailored, autism-specific education we’re proud to provide. We will provide updated information about the program as it becomes available.
Cooking Up Connections: The Magic of Family Time in the Kitchen

Parents are often looking for recommendations for fun family activities that could enrich their child’s life. Often, the best options can be found right at home.
Have you ever thought about involving your child in the kitchen? Activities such as preparing dinner, making a snack, or trying out a new recipe together can be a great start!

Cooking Skills and MORE
We all know that cooking teaches essential skills like measuring ingredients, following the sequence of steps in a recipe, and using various kitchen tools and equipment. Cooking provides an opportunity for children to learn how to handle utensils, chop vegetables, and stir batter. However, cooking offers far more than just the ability for your child to prepare meals for themselves and the family.
The kitchen is also an excellent place for sensory exploration – touching sticky textures (like dough) and experiencing various temperatures. Children with sensitivities to touch, taste, and smell, including those often described as "picky eaters," can benefit from this exposure, provided it allows them to explore at their own pace. This multi-sensory experience can expand their palate or help accommodate their specific support needs. For example, they may discover that wearing gloves can help their ability to handle certain textures.
The kitchen is not just a place for culinary adventures, it's also a classroom for safety. It's a perfect setting to teach children about the importance of being aware of extreme temperatures, sharp objects, breakables, and heavy items.
If you have concerns about kitchen safety, rest assured that there are kid-friendly tools like knives and scissors, non-slip cutting boards, and step stools available. You can gradually introduce them to heated tools, based on your and your child’s comfort level. This is also a great opportunity to demonstrate how to safely use the oven, stove, or air fryer.
The Beauty of Cooking at Home
One of the best things about cooking with your kids in the kitchen is that you can make this a space for them to explore, make mistakes, and learn in a safe and familiar environment. When things get messy, spills happen, hands get sticky, or something breaks accidentally, allowing them to experience the natural consequences, teaches cause and effect. Initially, holding back immediate corrective feedback and allowing them to do it themselves allows them to learn and adjust. This approach builds their confidence and kitchen skills and reinforces your role as a trusted adult they can rely on for guidance.
These moments in the kitchen become cherished family stories, offering a chance to share the joy of creating something. Children witness firsthand how to communicate and how cooperation leads to a delicious end product. When families cook together, they learn to work as a team.
As children grow more comfortable in the kitchen, they gain independence. Learning to prepare meals for themselves is an essential life skill throughout their lifespan. The confidence they earn from these experiences extends beyond the kitchen and may contribute to overall self-esteem. If cooking is an accessible skill for your child, there are benefits to starting early and introducing them to the kitchen, especially if this is an area of interest.
By making cooking a shared family activity, you not only impart essential life skills to your children but also create a nurturing environment. So, roll up your sleeves, grab those aprons, and enjoy the many rewards of cooking together!
---
Theresa is a Registered Occupational Therapist with experience working with children, youth, and adults with neurological differences in the private school, clinic, and community settings. She received her Doctorate Degree in Occupational Therapy from The University of Texas Medical Branch at Galveston. Prior to becoming an occupational therapist, she worked in the field of Applied Behavior Analysis as a Registered Behavior Technician. She is also a writer and consultant who offers her specialized knowledge to websites and companies serving the neurodiverse community.
Raising Independent Kids: Preparing for Life's Responsibilities

Throughout most of children's lives, parents wear the badge of caregiver. Not only do we coordinate our children's medical and mental healthcare, but we also pack lunches, pick out clothes, provide meals, and the list goes on. When you've spent so much time caregiving, it can be anxiety-provoking to start thinking about your child becoming independent and your role as a parent changing. However, isn't independence (to the greatest extent possible) the ultimate goal we want for all children?
Fostering independence has several long-term positive benefits for your child. We know it increases self-esteem and confidence, builds essential life skills, teaches the importance of completing a task, creates a sense of being part of a team, and ultimately helps establish a long-term pattern of self-help behaviors. The trick to fostering independence is to begin with the end in mind. What long-term goals do you have for your child? If your child is older, what are their goals? Are your expectations developmentally appropriate? Do your interactions with your child foster independence, codependency, or interdependence?
When we think about building a strong foundation for independence in the future, we think about a few key areas. Keep in mind that the pace at which your child masters these foundational skills will vary based on their individual abilities.
- Having developmentally appropriate expectations – It is important to ensure your child's expectations are not too low or too high. Think about your child's development in relation to their actual age.
- Practicing effective communication – Prioritize clear and calm communication, which is key to ensuring understanding and compliance. Give your child 5-10 seconds to respond to allow processing time. Utilize pictures and other visuals for communication if your child is a visual learner.
- Maximizing learning opportunities – Make daily activities into learning experiences by giving your child choices, narrating daily activities, letting your child help with tasks such as grocery shopping, and letting natural consequences happen when needed.
- Teaching self-care skills – Many of these tasks (ex: tooth brushing) often require several different steps that can be hard for children to understand and remember. Breaking self-care skills into smaller steps helps your child master one step at a time.
- Chores – These types of tasks are vital in building self-efficacy. Avoid chores that your child absolutely hates, as this will help set them and you up for success. Make sure that you teach proper techniques and avoid criticism whenever possible.
Over time, your child and family will master these foundational areas, at which point additional skills, such as planning, focusing attention, remembering instructions, and juggling multiple tasks, become essential to mastering higher-level learning. We call these mental processes "executive functioning," or what we fondly refer to as "the manager of the brain." As academic demands increase (usually around 3rd grade), you may begin to see your child struggle more in this area. You should speak with your child's school for ideas related to accommodations and supports.
As children enter adolescence, it is important for caregivers to starting thinking about independence in the context of their child navigating the world around them. These tips can help your child build independence in the areas of everyday life, school, and their medical care.
- Foster critical thinking – Do not just give your child the answers when they ask you a question. Instead, ask: How do you think we should do that? Where do you think that can be found?
- Teach emergency response – Model and practice handling scenarios at home, such as a fire, a burglary, a medical emergency, etc.
- Talk about the future – Ask your child what they are interested in and prompt conversations about their goals for the future.
Include your child in school meetings (to the extent possible) – Children should know their accommodations and supports and be able to express (verbally or non-verbally) any new needs that may arise. - Prepare them for social settings – Practice common social situations at home such as using lockers, changing in gym, responding to bullying, etc.
- Familiarize them with medical and mental health areas – Children should know what types of doctors they see and why they see them (including the extent of those relationships). They should also know what medications they take and why they are taking them. Do not shy away from topics such as puberty, sexuality, and relationships. It is better for your child to hear these things from you than from a friend.
Developing independent life skills is not a linear process. It is normal for children and teens to take two steps forward, one step back, and then two more steps forward again. Praise progress often, and do not be discouraged! Fostering independence for your child is a marathon, not a sprint.
---
Jennifer Cervantes, LCSW-S, and Dinah Godwin, LCSW-S are Licensed Clinical Social Workers at Meyer Center for Developmental Pediatrics and Autism and Assistant Professors in the Department of Pediatrics at Baylor College of Medicine with extensive experience supporting families of children with developmental disabilities. Jennifer has over a decade of experience in school social work, foster care, and trauma-informed care, while Dinah brings more than 20 years of expertise in clinical care, caregiver support, and program development. Both are passionate about positive behavior management, advocacy, and empowering families through education and community resources.
This blog post was adapted from the presentation given during WestviewEDU on Thursday, March 5, 2025. WestviewEDU is an education series presented by The Westview School for parents and caregivers of children with autism spectrum disorder. For a complete list of WestviewEDU sessions remaining for the 2024-2025 academic calendar year, visit The Westview School online.